
Systematic cueing should be provided for those with dementia to complete the walk tests. Practice effect associated with the walk tests was found within and across testing occasions for frail older adults with normal cognition, and only within the same testing occasion for those with dementia. Multivariate regression analyses showed that the cognitive function of the DEM group was independently and inversely associated with the level of cueing provided during the walk tests ( p ≤ .007).
Significant increases in the walking performance across testing occasions were shown in the 2MWT ( p ≤ .047), 6MWT ( p ≤ .005) and 10MeWT ( p ≤ .039) for the NON-DEM group but not the DEM group (all p > .05). Significant increases in the walking performance within the same testing occasion were found in the 2MWT (NON-DEM: p = .002 DEM: p ≤ .044) and 6MWT (NON-DEM: p ≤ .004 DEM: p ≤ .002) for both groups but only in the 10MeWT ( p ≤ .023) for the DEM group. The DEM group was facilitated to complete the walk tests using a progressive cueing system. A similar approach in vertebral fragility fractures might also deliver improved outcomes.ġ) To determine if there was a practice effect associated with walk tests performed by frail older adults with and without dementia, 2) to examine the role of systematic cueing in the walk tests for those with dementia, and 3) to make recommendations to testing protocols of the walk tests for frail older adults with and without dementia.Ĥ4 frail older adults with normal cognition (NON-DEM) and 39 older adults with Alzheimer's disease or dementia (DEM) who were able to walk independently for at least 15 m.Īll the participants completed multiple trials of 2-minute walk test (2MWT), 6-minute walk test (6MWT) and 10-meter walk test (10MeWT) on three separate testing occasions. Quality standards and re-organising care in hip fracture has led to improved outcomes. Many did not receive adequate pain relief and appropriate assessments to reduce their future fall and fracture risk. Improvements could be made to hospital vertebral fracture care. On discharge, 76% still required opioids and only 56% had a plan for their bone health. While in hospital, 31% developed a medical complication, with infection being the most common one. Despite many in severe pain, only a third were prescribed opioids with the median dose of morphine-equivalent was 10-20 mg daily for the first three days of admission. 9% proceeded to have vertebral augmentation. Many patients on medical wards had input from spinal surgical team and vice versa. Patients cared for by medical teams were older, frailer, had a higher prevalence of cognitive impairment, more dependent for daily living and less mobile compared to those under the care of the spinal surgical team. 46% or patients were managed on geriatric medicine wards, 39% on general medical wards, and followed by 14% on spinal surgical wards. There was variation in the content of the radiology reports. X-ray of the spine was the most common imaging of choice to diagnose a fracture. 38% had a concomitant medical diagnosis, such as an ongoing infection. 69% presented to hospital 24 h after the onset of their severe acute back pain. Information was collected from patients and electronic health records on their presentation and hospital care.ĩ0 patients were recruited into the study. This was an observational study of adults aged 50 years and over admitted to hospital over 12 months with an acute vertebral fragility fracture. This study aimed to describe the hospital treatment received in one UK university hospital with the purpose of proposing what hospital services should look like. Patients that require hospital admission for vertebral fragility fractures were older, multimorbid, frail, have cognitive impairment and were in severe pain.

Further evaluation of the scale is recommended to assess its validity in other units, and to assess its predictive validity for discharge outcome and physiotherapy outcome. The EMS provides physiotherapists with a standardised validated scale for assessment of frail elderly people and was designed to be used in conjunction with the assessment package recommended by the Royal College of Physicians and British Geriatric Society (1992).
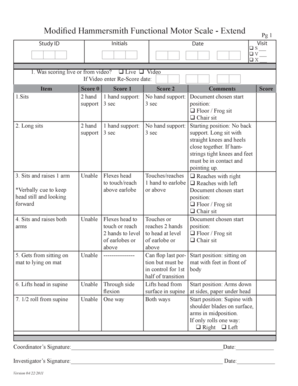

There was no significant difference between scores. Inter-rater reliability was established on 15 patients who were assessed independently by two physiotherapists. Spearman's rho was 0.962 with Barthel and 0.948 with FIM - highly significant correlations. Concurrent validity was established by correlating the Elderly Mobility Scale (EMS) score with Barthel and functional independence measure (FIM) scores for 36 patients, age 70–93 years. This study established the concurrent validity and inter-rater reliability of a simple mobility scale for frail elderly people.


 0 kommentar(er)
0 kommentar(er)
