

The primary objective in this study was to evaluate the trends for postoperative complication rates over a 7-year period (2012–2018). However, studies assessing this issue in general across multiple subspecialties and thereby estimating the overall extent of postoperative complications and its trend over time are lacking.
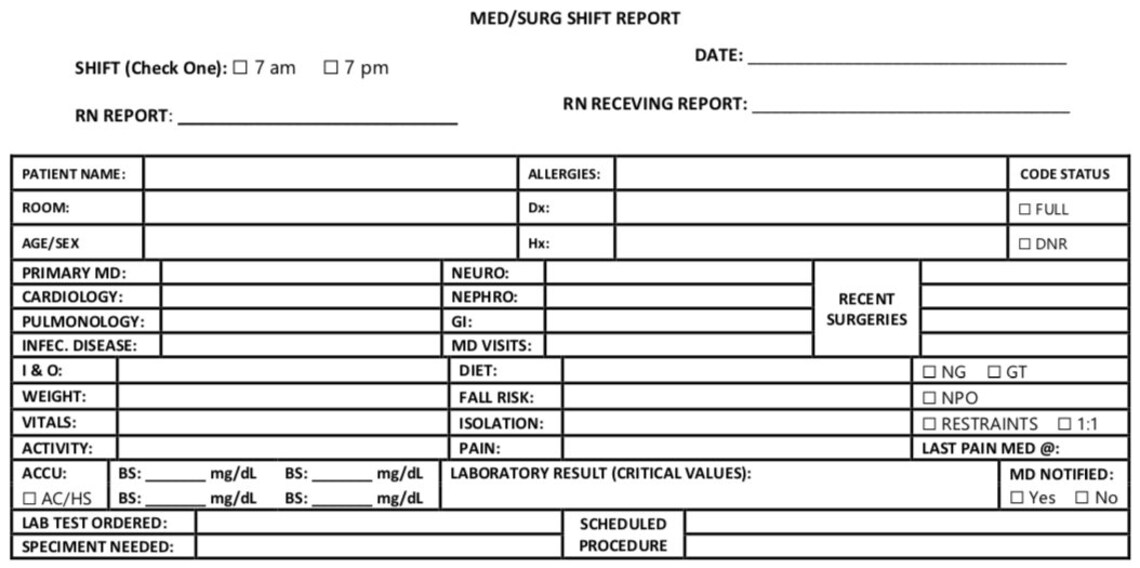
#PATIENTS SURGERY REPORT FILE PC#
PC trends following total knee arthroplasty (TKA) has been reported to decrease during a 10-year study period (2006–2016). Ī number of studies have highlighted the scope of the problem within specific surgical subspecialties. From a societal standpoint, PCs account for a large financial burden in the form of additional health care expenses when a patient requires Intensive Care Unit (ICU) treatment, reoperation or readmission, thereby increasing healthcare costs in an estimated order of magnitude between $11,626 and $19,626 in additional healthcare expenses per patient. In the individual level, PCs can have major impact on the individual patient, potentially resulting in a decline of both quality of life as well as functional performance. According to the Clavien-Dindo classification, a PC is defined as any deviation from the normal postoperative course, meaning that the severity ranges from non-life-threatening complications with no lasting disability to fatal outcomes. Furthermore, the overall postoperative mortality rate is reported to vary from 0.79 to 5.7%. Studies estimate that 7–15% of patients undergoing major surgery will experience a postoperative complication (PC). The total volume of major surgeries performed annually worldwide was estimated to be 312.9 million in 2012-an increase of 38.2% from 2004. Incidence rates for the complications exhibited a stable trend over the study period, with minor in or decreases observed. However, OR’s for organ/space SSI 1.05, myocardial infarction 1.01 and sepsis 1.01 increased slightly over time (all p < 0.01). When adjusted, regression analyses indicated decreased odds ratios (OR) through the study period years for particularly deep SSI OR 0.92, superficial SSI OR 0.94 and acute renal failure OR 0.96 as the predictor variable (study year) increased (p < 0.01). Incidence rate for organ/space SSI exhibited an increase (1.1 to 1.5%).

Particularly the incidence rates of four complications were found to be decreasing: superficial SSI (1.9 to 1.3%), deep SSI (0.6 to 0.4%), urinary tract infection (1.6 to 1.2%) and patient unplanned return to the operating room (3.1 to 2.7%). ResultsĪ total of 5,880,829 patients undergoing major surgery were included. Multivariable logistic regression was used to associate complication rates with dataset year, while adjusting for relevant confounders. The NSQIP datasets from 2012 to 2018 were used to assess 30-day complication incidence rates including mortality rate following surgical procedures within ten surgical subspecialties. The objective of this study was to evaluate the trends of postoperative complication rates over a 7-year period. Postoperative complications continue to constitute a major issue for both the healthcare system and the individual patient and are associated with inferior outcomes and higher healthcare costs.


 0 kommentar(er)
0 kommentar(er)
